Mixed neuroendocrine tumors of the middle ear (MeMeNET), previously middle ear adenomas or middle ear carcinoids, are rare middle ear neoplasms that very rarely exhibit skull base invasion and malignant potential. However, we present a unique case of locally recurrent and metastatic MeMeNET with skull base involvement and facial nerve paralysis.
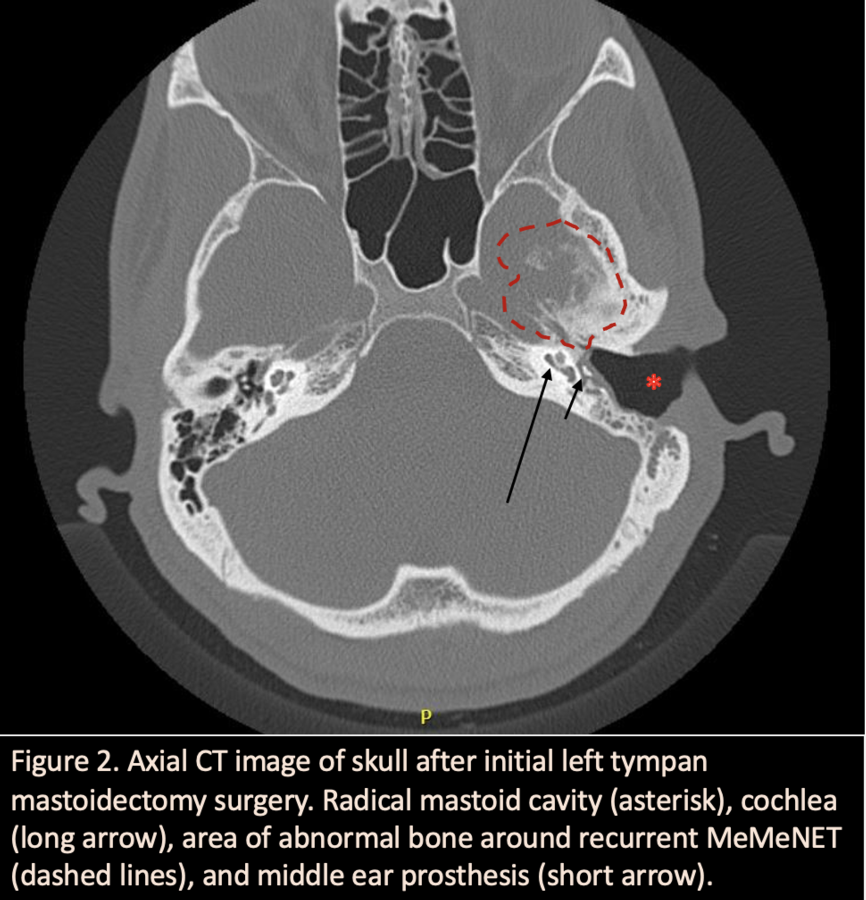
A 31-year-old male was referred to our clinic with 1 month of left-sided facial weakness, otalgia, and hearing loss refractory to aggressive antibiotics and steroids. Physical exam revealed left-sided facial paresis House-Brackmann V/VI; otologic exam showed a mass emanating from middle ear, obliterating the tympanic membrane, and extending to ear canal. Computed tomography (CT) showed a soft-tissue density filling the middle ear and mastoid. Bony structures were preserved despite being in contact with the mass. Given the facial nerve paresis, urgent transmastoid facial nerve decompression with biopsy of the mass was performed.
Specimens were originally interpreted as low to intermediate grade neuroendocrine neoplasms, or middle ear adenomatoid tumors (MEANT). Given the benign pathology, gross total resection was achieved, and the ear drum and ossicular chain were reconstructed. The patient regained complete facial nerve function within 2 weeks of surgery.
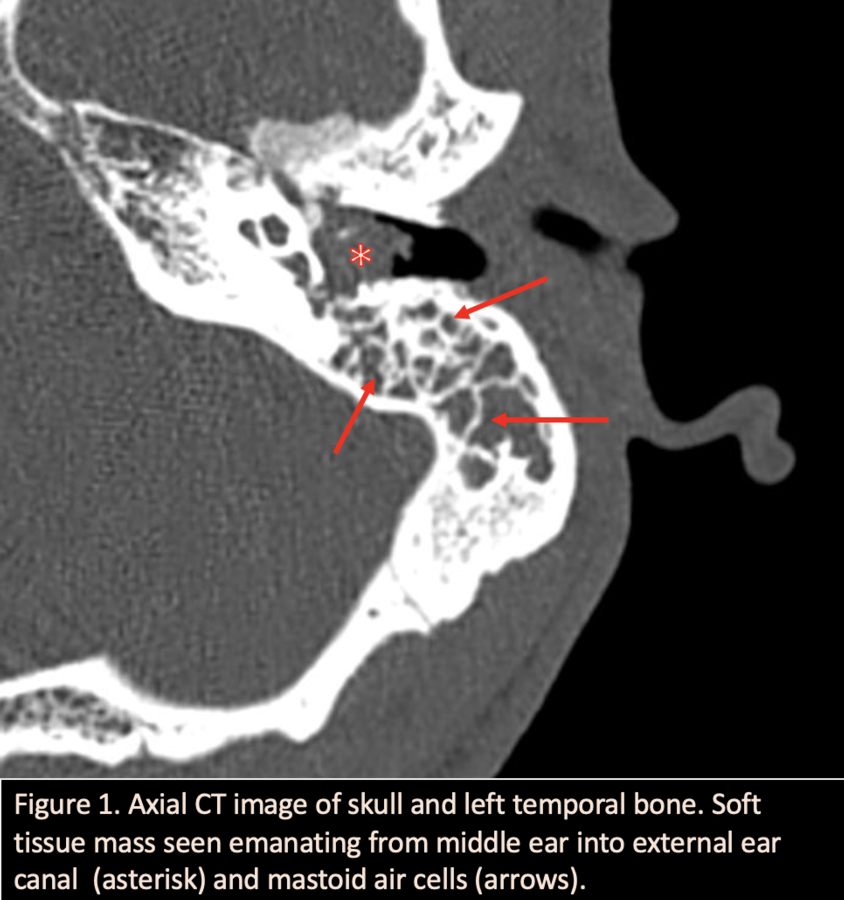
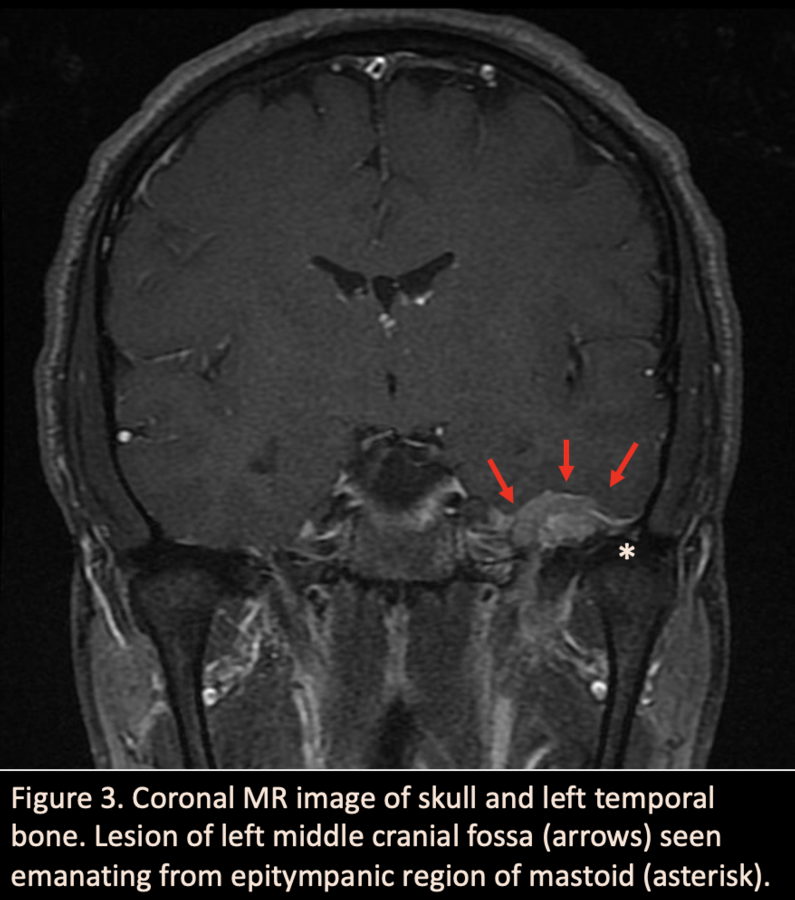
Unfortunately, he returned 6 months later with new onset subjective aural fullness. New imaging revealed recurrence in the mastoid and erosion of the tegmen with 2.1cm mass extending up into the middle cranial fossa. Tumor board recommendation was aggressive surgical resection which included combined middle fossa craniotomy and lateral temporal bone resection. The tumor was found extensively infiltrating the tegmen tympani and middle fossa dura.
Re-evaluation of the pathology specimens at different institutions around the country revealed mixed opinions and was ultimately was diagnosed and reclassified as MeMeNET. Metastatic workup revealed revealed a 2-cm lesion between the medial and lateral pterygoid muscles and multiple liver foci which were biopsy confirmed as MeMeNET via immunohistochemical staining. The patient underwent targeted proton radiation for the pterygoid lesion and everolimus for his liver metastases. At this time, the patient maintained excellent facial nerve function and no sign of local recurrence.
This case draws attention to the recent re-classification of middle ear adenomas as potentially malignant MeMeNETs. Skull base surgeons need to be aware of this reclassification which directs clinical management including metastatic workup, aggressive radical surgery, and likely post-operative radiation.
Complete surgical removal is considered optimal treatment for primary and metastatic lesions, though there is no standard approach given its rarity. Adjuvant radiotherapy has been documented in some cases, though some hypothesize radiation my induce malignant transformation. A curious yet concerning feature of this neoplasm is the clinical finding, and resolution, of facial nerve palsy. While locally destructive to middle ear structures, full facial nerve function returned upon tumor resection. Though MeMeNETs typically remain benign, this case contributes to literature surrounding the possibility for local malignant invasion, distant metastasis, and prognostic indicators.