Background: Rathke's cleft cyst (RCC) is a benign sellar or suprasellar lesion often discovered incidentally. Often, lesions do not grow on subsequent imaging, are asymptomatic, and are treated conservatively. When symptomatic, patients will often present with refractory headaches, visual disturbances, and occasionally hypopituitarinism. Occasionally, patients present with meningismus, fever and other clinical signs of meningitis. We present a case of a patient with recurrent aseptic meningitis with an enlarging RCC with surgical pathology consistent with secondary hypophysitis. An additional literature review of RCC associated hypophysitis cases was performed.
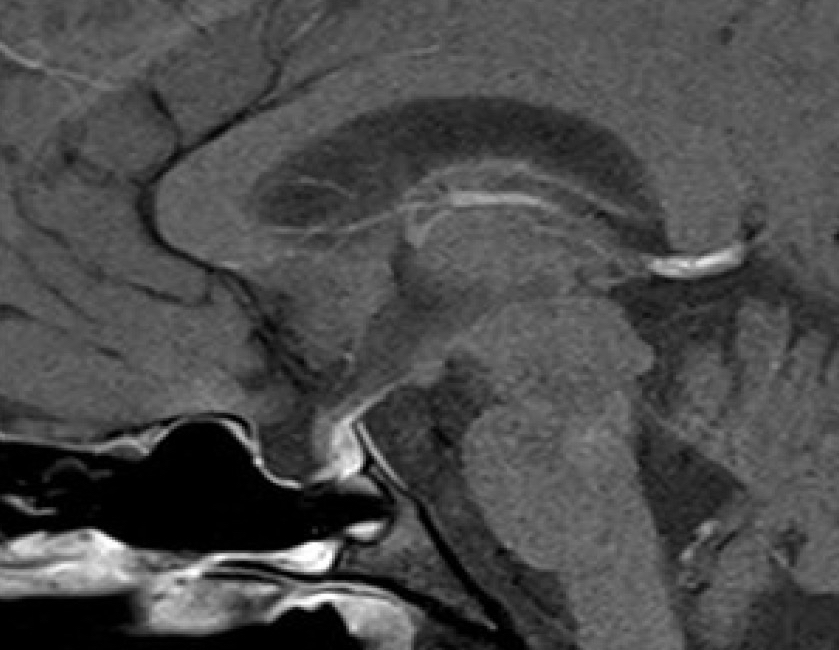
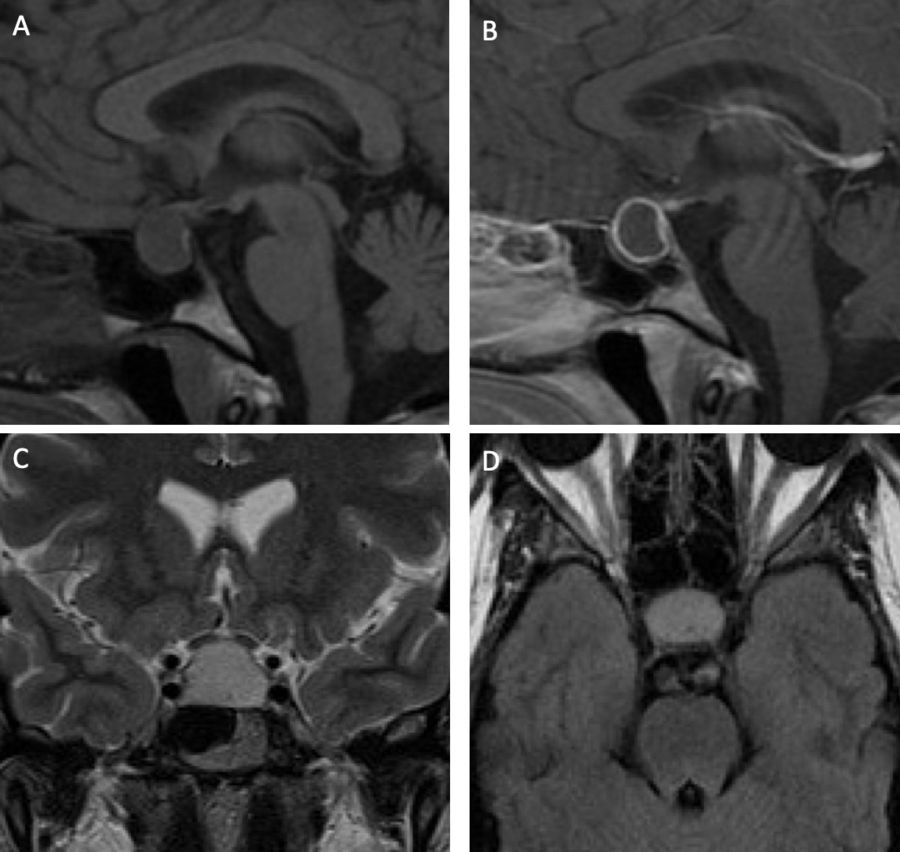
Case: A 30-year-old female presented with three episodes of intractable headaches in the span of two 8 weeks. During each episode, her clinical presentation was consistent with meningitis, for which she underwent repeated lumbar punctures. No bacteria or viruses were ever isolated from cerebrospinal fluid and antimicrobial therapy was withheld. Intracranial imaging revealed a cystic sellar lesion, initially thought to be unrelated (fig 1A-D). On her third presentation, repeat MRI demonstrated interval rapid enlargement of the cyst with suprasellar extension, significant compression of the optic chiasm, and enhancement extending into the basal frontal lobes (fig 2A-C). The patient was taken for resection via an endoscopic transsphenoidal approach. Intraoperatively, mucopurulent material drained from the cyst and the cyst wall was resected. Final pathology demonstrated ciliated epithelium with focal squamous metaplasia with surrounding acute and chronic inflammation suggestive of RCC with hypophysitis. No definitive organism was isolated from intraoperative cultures. Postoperative MRI demonstrated complete resolution of the cyst (fig 3).
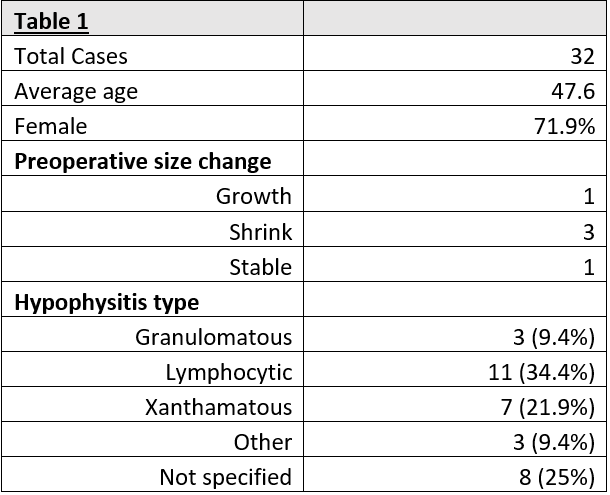
Discussion: We present here a patient with 8 weeks of recurrent aseptic meningitis with a Rathke's cleft cyst initially managed conservatively until subsequent rapid lesion growth and worsening symptoms prompted surgical evacuation. The presumed pathophysiology is rupture of the RCC triggering a potent immune response. This is supported by her recurrent meningitis symptoms with sterile CSF cultures. A literature review of RCC associated hypophysitis cases returned 32 cases with a mean age of 47.6 years and a female predominance (71.9%). The most common final histopathologic diagnosis was lymphocytic hypophysitis (34.4%) followed by xanthamatous (9.4%) and granulomatous (9.4%) hypophysitis (table 1). Our patient's presentation was unusual based on an 8-week time course and rapid growth of her lesion. Of the 32 identified cases of RCC associated hypophysitis in the literature, only 1 other case demonstrated interval growth prior to surgical intervention. It demonstrates the importance of re-imaging these patients when the clinical picture worsens.
Conclusion: Secondary hypophysitis from a Rathke's cleft cyst is a rare presentation that can be difficult to diagnose. Our case demonstrates the unusual presentation of a rapidly enlarging RCC requiring surgical evacuation. It's important to keep ruptured RCC in the differential of symptomatic cystic sellar lesions.
.jpeg)