Background: Solitary extramedullary plasmacytomas (EMPs) are nonepithelial neoplasms of plasma cell origin categorized among non-Hodgkin lymphomas, without bone marrow involvement or systemic spread. EMPs are uncommon tumors comprising only 3-4% of all plasma cell neoplasias and represent 1% of head and neck tumors. Approximately 80% of EMPs occur in the upper respiratory tract with an 11-33% conversion rate to multiple myeloma in 10 years. The authors could only locate 2 cases of EMPs localized to the frontal sinus reported in the literature.
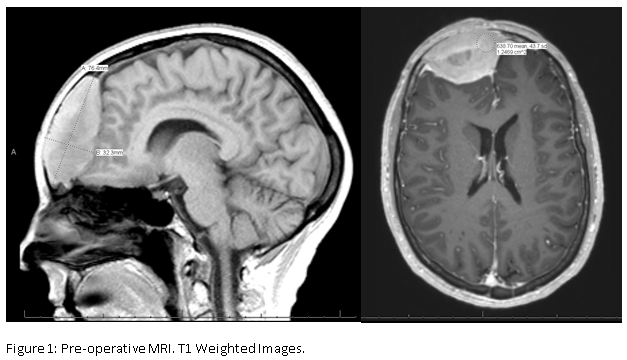
Case Presentation: We present a rare case of a 60 year old asymptomatic female who presented to her primary care physician after noticing a pulsatile erosion in the frontal bone of her skull. At the time of presentation, the patient denied any other neurological or obstructive symptoms.60 year old asymptomatic female who presented to her primary care physician after noticing a pulsatile erosion in the frontal bone of her skull. At the time of presentation, the patient denied any other neurological or obstructive symptoms.The patient underwent magnetic resonance and computed tomography imaging, which revealed a 7 x 7 x 3 cm mass in her frontal sinus compressing the frontal lobe of her brain (Fig 1).
Management/Outcome: The patient underwent resection and Medpor cranioplasty with pericranial flap obliteration of her frontal sinus. During the resection, it was noted that the mass did not violate the dura allowing for a complete resection of the mass. Histopathology was positive for CD 138 and had kappa light chain restriction consistent with plasmacytosis. The patient underwent further hematologic workup with bone marrow biopsy and PET/CT without findings concerning for myeloma. With complete resection of the plasmacytoma, the decision was made that the patient did not require adjuvant radiotherapy. Follow-up MRI indicated complete resection of the plasmacytoma (Fig 2). PET/CT confirmed that there as no residual disease or additional foci of disease. The patient has remained symptom and disease free at this time. The patient will undergo hematological monitoring with hematology-oncology every 4 months and a follow-up MRI will be obtained 6-months postoperatively to monitor for progression of disease.
.PNG)
Conclusions: The clinical presentation of paranasal sinus EMPs depends on volume of the mass and site of involvement. The tumor is slow-growing in nature and patients only become symptomatic once the mass completely fills the sinus cavity. In the rare case presented, the patient was asymptomatic at time of presenation, however, EMPs are generally are diagnosed after the patients present to their physician with symptoms of nasal obstruction, soft-tissue swelling, epistaxis, nasal discharge, pain, and proptosis, observed in decreasing order of frequency. While this is a rare condition, EMPs should always be considered when forming a differential diagnosis in older patient's presenting with head and neck tumors or symptoms of nasal blockage/abnormal nasal discharge. EMPs have a reported conversion rate to multiple myeloma of 11 - 33% making long term follow up mandatory even if the decision is made to pursue adjuvant radiotherapy.