Background: The retrosigmoid suboccipital craniotomy is a commonly used surgical corridor to the cerebellopontine angle. Despite its frequent utilization among neurosurgeons, there remains no standardized repair technique for this craniotomy. The risks of this approach include post-operative CSF leak, persistent suboccipital headaches, and wound infections. We report our institutional experience performing a multi-layered anatomic repair of the retrosigmoid suboccipital craniotomy.
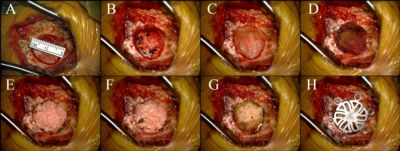
Methods: A retrospective chart review was performed in twenty-five consecutive patients that underwent retrosigmoid suboccipital craniotomy, to evaluate for incidence of post-operative headache, CSF leak, or wound infection. All patients underwent a retrosigmoid approach in the lateral “park bench” position, using a linear incision within the hair-bearing scalp. A 14-18mm craniectomy was performed using a high-speed drill, with bone dust saved in antibiotic saline for subsequent repair (figure 1A). Any exposed mastoid air cells were obliterated with bone wax during the approach and again prior to final repair. The dura was opened in a C-shape and reflected laterally towards the transverse sinus. After completing the intradural portion of the operation, the dura was primarily repaired using interrupted 4-0 braided nylon suture (figure 1B). A collagen on-lay was then placed on top of the dural repair (figure 1C), followed by Surgicel (Ethicon) (figure 1D), then autologous bone chips/dust from the craniectomy (figure 1E and 1F), followed by a second outer layer of Surgicel (Ethicon) to secure the bone in place (figure 1G). A titanium burr hole plate was then placed over the entire defect (figure 1H). Muscle layers were reapproximated individually using 3-0 vicryl sutures. The deep fascia and dermis were reapproximated using 3-0 vicryl sutures, and a simple running 4-0 nylon suture was used to close the skin. The wound was dressed with bacitracin ointment, a non-adhesive gauze covering, and tape. Dressings were left in place for 48hrs, then patients were instructed to shower daily and apply no ointments to the incision.
Figure 1 - Panel A-H depict a step by step demonstration of the cranioplasty technique describe in this abstract.
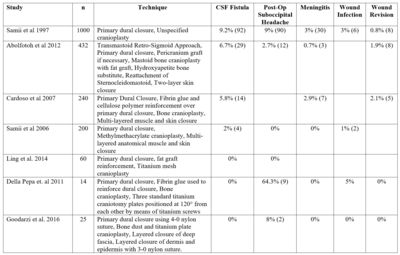
Results: A consecutive series of twenty-five patients with a mean follow-up time of 16 months was included in this study. Of the 25 patients retrospectively reviewed, two patients (8%) reported persistent suboccipital headaches. None of the patients in this series developed CSF leak or wound infections. Outcomes were similar to those reported in previous clinical series (Table 1).
Table 1 - A list of techniques utilized for the repair of the retrosidmoid suboccipital craniotomy and their associated complication rates.
Conclusion: A multi-layered anatomic repair after retrosigmoid suboccipital craniotomy results in favorable clinical results and may reduce the risks associated with this operation.